Considerations for
Exercise Therapy
“Patients with long COVID asked for rehabilitation. Many of them, including previously healthy and fit clinicians, tried to fight postviral fatigue with exercise-based rehabilitation. We observed a growing number of patients with long COVID who experienced adverse effects from exercise therapy and symptoms strikingly similar to those of myalgic encephalomyelitis (ME). Community-based physical therapists, including those in private practice, unaware of safety issues, are preparing to help an influx of patients with long COVID.”
– Journal of Orthopaedic & Sports Physical Therapy
Post-Covid Physical Therapy
- Post-Covid Conditions & Long Covid
- Screening & Assessment
- More on Post-Exertional Malaise (PEM)
- The Harm of Graded Exercise Therapy
- Guidance from Experts
This page is specifically intended for physical therapists. All information provided on and through this website is provided for informational purposes only.
89.1% of Covid Long Haulers experience PEM and are at risk for a worsening of their condition due to “pushing through” symptoms or going beyond their personal limits. For some, this worsening can be permanent.
“More than 3 decades otrying exercise in this population can be summed up in one sentence: exercise can be harmful, sometimes life threatening, and should be avoided.”
– Journal of Orthopaedic & Sports Physical Therapy
1. Post-Covid Conditions & Long Covid
“Long Covid” is used to describe Post-Covid medical conditions, IE: post-acute sequelae SARS-CoV-2 infection (PASC).
Acute COVID-19 severity does not necessarily predict subsequent or ongoing symptoms.
Long Covid is not rare.
The CDC is reporting that 1 /5 of adults who contract COVID will develop a Post-Covid Condition.
The American Academy of Pediatrics states that Long Covid is affecting children and adolescence and references United Kingdom Office for National Statistics estimate:
– 12.9% of children 2 to 11 years of age
– 14.5% of children 12 to 16 years of age
still experienced symptoms 5 weeks after infection.
All patients who test positive for a SARS-CoV-2 infection should have at least one follow-up appointment with emphasis on cardiac symptoms.
– The American Academy of Pediatrics
2. Screening & Assessment
Special considerations when working with patients with Long COVID:
- Cardiac Inpairment
- Oxygen desaturation
- Orthostatic Intolerance & Dysautonomia
- Post-Exertional Malaise
Cardiac Impairment
“Exclude cardiac impairment before using physical activity (including exercise or sport) as rehabilitation interventions for people living with Long COVID, with continued monitoring for potential delayed development of cardiac dysfunction when any physical activity interventions are commenced.”
– World Physio Therapy Safe & Effective Rehabilitation – Briefing Paper 9, Pages 10 & 11
*** CARDIAC WARNING ***
Cardiac symptoms require further clinical assessment, and may indicate the need to stop and seek medical advice. Mild cardiac impairment has been found in significant portions of those with Long COVID and warrants evaluation and extreme caution.
Cardiac impairment in Long Covid >
Oxygen Desaturation & Hyperventilation
“Exclude exertional oxygen desaturation before using physical activity (including exercise or sport) as rehabilitation interventions for people living with Long COVID, with continued monitoring for signs of reduced oxygen saturation in response to any physical activity interventions.”
– World Physio Therapy Safe & Effective Rehabilitation – Briefing Paper 9, Pages 11 & 12
Caution & further investigation is warranted for patients who experience:
- A fall in oxygen of 3% or more with exertion is considered abnormal and should be further investigated.
- Hyperventilation syndrome and breathing pattern disorders have been observed in those with Long COVID.
Orthostatic Intolerance & Dysautonomia
“Autonomic dysfunction, presenting as breathlessness, palpitations, fatigue, chest pain, feeling faint (presyncope) or syncope, could contribute to the exercise intolerance observed in people with Long COVID. Safe administration of physical activity interventions for individuals with Long COVID will require informed clinical decision making, carefully designed care plans, and consistent symptom monitoring.“
– World Physio Therapy Safe & Effective Rehabilitation – Briefing Paper 9 Page 12
Orthostatic Intolerance
What is it?
Orthostatic intolerance refers to the inability to maintain an upright posture. Patients may experience a light-headedness, dizziness, nausea, leg pain, and breathlessness.
Dysautonomia is an umbrella term that describes several different conditions that cause a dysfunctioning of the Autonomic Nervous System which controls the “automatic” functions of the body:
- Heart rate
- Blood pressure
- Digestion
- Dilation and constriction of the pupils of the eye
- Kidney function
- Temperature control
Common forms of Dysutonomia diagnosed after COVID infection are Postural Orthostatic Tachycardia Syndrome (POTS) & Orthostatic Hypotension (sometimes referred to as Neurally Mediated Hypotension or NMH.)
Commonly seen in Long COVID
Orthostatic Intolerance and Dysautonomia is a common complication of Long COVID, with a recent study suggesting that 67% of Long COVID patients experience autonomic nervous system dysfunction, despite the severity of their acute COVID-19 infection.
In office assessment for Dysautonomia
Measurement of blood pressure and heart rate while resting supine and every minute for 10 min while standing with shoulder-blades on the wall for a relaxed stance.
Management
Management techniques that are commonly suggested for Dysautonomia have been largely adopted by the Long Covid community.
- Compression gear
- Electrolyte drinks
- Heat avoidance
- Shower chairs
- Mobility aids
- Heart rate monitors
- Blood pressure monitors
- Avoid standing for long periods
Our Dysautonomia Research & Resource Collection >
Post-Exertional Malaise
“Before recommending physical activity (including exercise or sport) as rehabilitation interventions for people living with Long COVID, individuals should be screened for post-exertional symptom exacerbation through careful monitoring of signs and symptoms both during and in the days following increased physical activity, with continued monitoring in response to any physical activity interventions.”
–World Physiotherapy response to COVID-19, Briefing paper 9
PEM can be extremely difficult for patients to identity since the symptom onset, or crash, is usually delayed by hours or days. Simply asking patients if they have PEM is not sufficient.
- Patients may describe:
- A crash, relapse, collapse after physical activity
- Being mentally tired after the slightest effort
- Being physically drained or sick after mild activity
- The more demanding, prolonged or repeated the activity, the more severe and prolonged the payback
- Questionnaires:
- RAND-36 (fast clinical version of the SF-36)
- Good/Bad Day Questionnaire
- DePaul Symptom Questionnaire (recommended 1st step by National Institutes of Health, NIH & Centers for Disease Control, CDC)
- Health Assessment Form
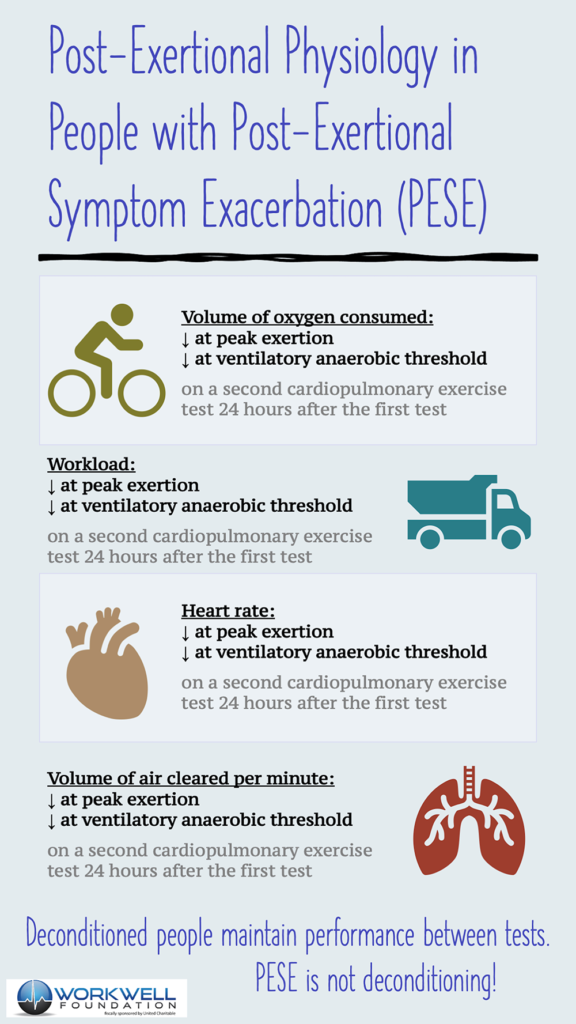
- Two-day CPET testing
!!!! use with caution, as this may induce severe PEM symptoms and permanent consequences !!! - Guided provider questions
- “What happens when you engage in normal (previously tolerated) physical or mental exertion?”
- “How much activity does it take to make you feel ill or to trigger illness worsening?”
- “How long does it take to recover from physical or mental effort?”
- “Do you avoid or change certain activities because of what happens after you do them?”
3. More on Post-Exertional Malaise (PEM)
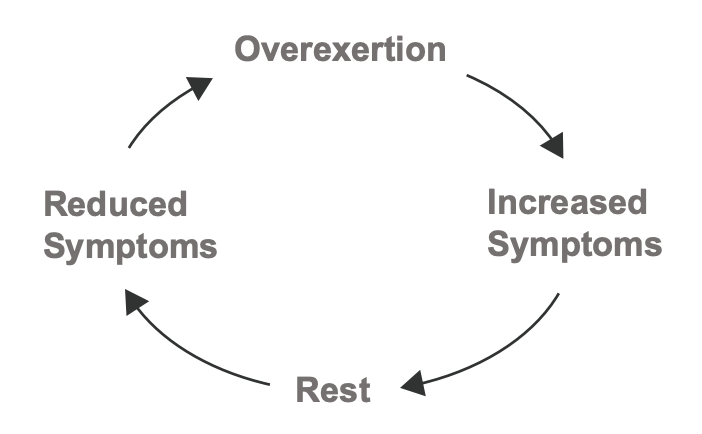
Post-Exertional Malaise, or PEM is an abnormal physiological response to physical or cognitive exertion. PEM is a key symptom of myalgic encephalomyelitis (ME) and chronic fatigue syndrome (CFS) and like other neurological diseases, up to 80% of cases of ME/CFS are initiated by infection. Estimates are showing that ~50% of Covid Long Haulers will meet the criteria for ME/CFS.
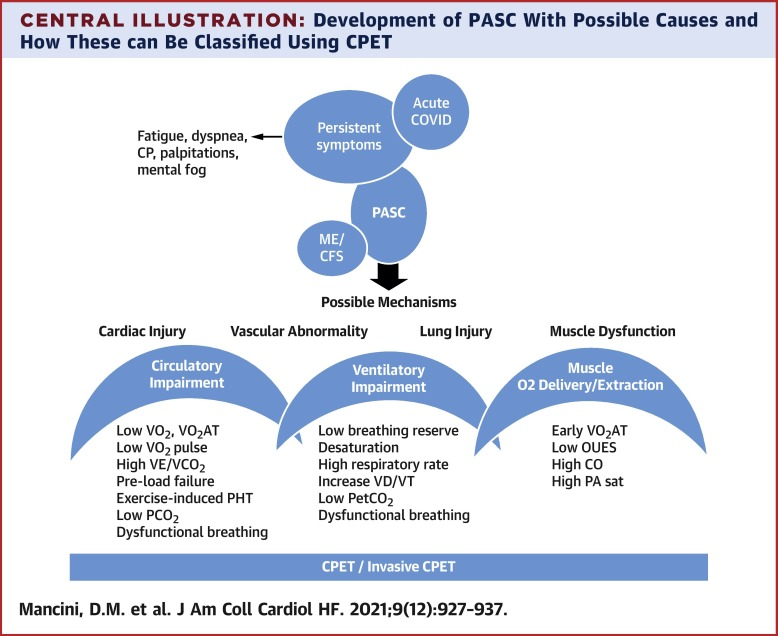
Physiological differences in Long Haulers experiencing PEM can be measured with Cardiopulmonary Stress Testing, or CPET. In November 2021, Use of Cardiopulmonary Stress Testing for Patients With Unexplained Dyspnea Post–Coronavirus Disease, identified abnormal findings in: circulatory impairment, abnormal ventilatory pattern, dysfunctional breathing, and resting hypocapnia.
Key Concepts
PEM can be triggered after daily activities:
a shower, a phone call, or a walk around the block. Everyones threshold is different and can vary.
The PEM “crash” can feel like the flu, an increase in neurological symptoms, gastrointestinal symptoms, headaches, sensory sensitivity, or crushing fatigue.
The crash can persist for hours, days, weeks, or permanently.
PEM symptoms are usually delayed. Onset is a worsening symptoms, usually delayed by hours or days.
PHYSICAL CONDITIONING
Exercise intolerance observed in Long COVID is not physical deconditioning. There is important physiological differences in response to acute exercise between people with deconditioning compared to people with PEM and Long COVID.
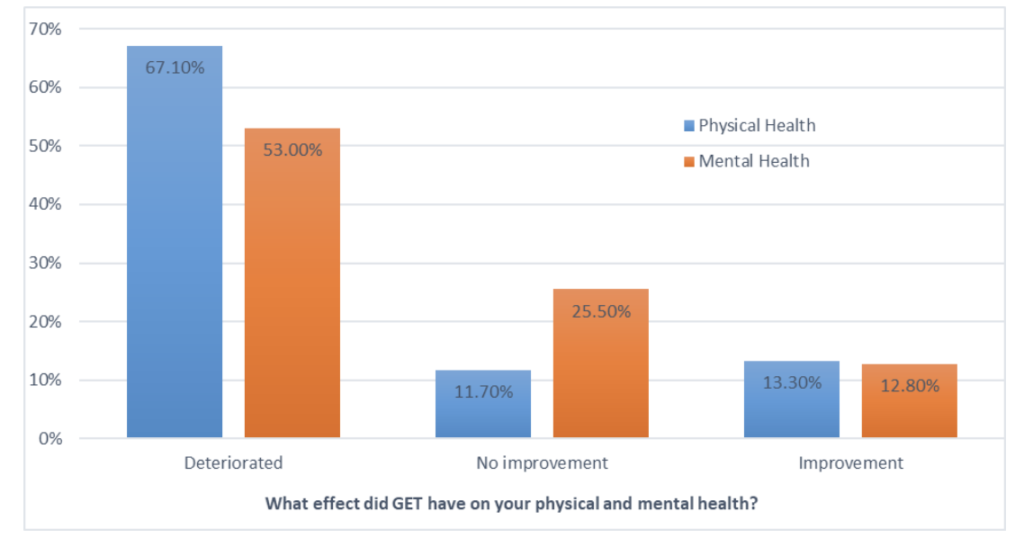
4. The Harm of Graded Exercise Therapy
Graded exercise therapy, or GET, is a form of physical therapy where physical activity is gradually increased over time, regardless of how the patient is feeling and ignoring any increased symptoms or new symptoms.
GET is also known as Graded Activity Management (GAM), and Graded Activity Therapy (GAT).
G.E.T. has been found as harmful to the majority of patients
“Our review shows that more patients are unable to work after treatment with CBT and GET, than before treatment with it.”
– Healthcare 2022
“The GET recommendation was removed by the 2021 NICE guidelines update because of high rates of harm.”
– MEPedia
Forward ME and Oxford Brookes University Patient Survey
participated in CBT and GET interventional
“NICE’s 2019 patient survey: 13% presented with severe ME before doing GET treatment which increased to 35% with severe ME after GET treatment.”
– MEPedia
Prevent Decline
The average person with ME/CFS scores as more disabled on quality of life surveys than those with multiple sclerosis, stroke, diabetes, renal failure, lung disease, heart failure, and cancer.
5. Guidance from Experts
World Physio Therapy
Safe & Effective Rehabilitation Briefing Paper 9
Key Points
- Individualized for each patient
- The goal is to stabilize symptoms
“Aiming to achieve sustainable symptom stabilization, whereby symptom fluctuations are reduced to a manageable level over a period of time, can constitute a rehabilitation approach that improves symptom severity and daily functioning.”
Overview of the Briefing Paper
The Bateman Horne Center
“An important role for the medical provider is to teach patients about PEM and how to manage through pacing. Pacing is an individualized approach to managing physical, cognitive, and emotional energy within a patient’s specific limits by carefully planning where and how to spend their available energy. Pacing is a critical tool to prevent and/or reduce PEM.”
- Ideally, the patient should only engage in the amount of activity that doesn’t induce PEM in 24-48 hours. The goal is to get back to “baseline” the following morning. If PEM is induced, rest is required until it resolves.
- Help the patient develop a heightened sense of awareness about the threshold of relapse and the consequences of moving beyond their envelope.
- Activity logs, heart rate monitors, smart watches, and the Oura Ring are all helpful tools to give immediate/daily/weekly/monthly feedback on activity and pacing.”
More from Bateman Horne Center – Guidance for Clinicians >
More Resources:
Breathing Exercise with Stasis >
Autonomic Conditioning Therapy (ACT) for PACS (used Stasis) >
CDC Guide for Managing PEM >
Continuing Education >
LONG HAULERS please STOP.REST.PACE from MEACTION.NET
COMMUNITY SUPPORT
Long Covid Families is happy to support the community in any way we can. Join our Facebook Support Group, follow us on social media, or contact us, anytime.
SUPPORT THE CAUSE
Donations are tax deducible and every little bit helps us pay for the essential tools we use for advocacy & awareness. Donate to Long Covid Families.